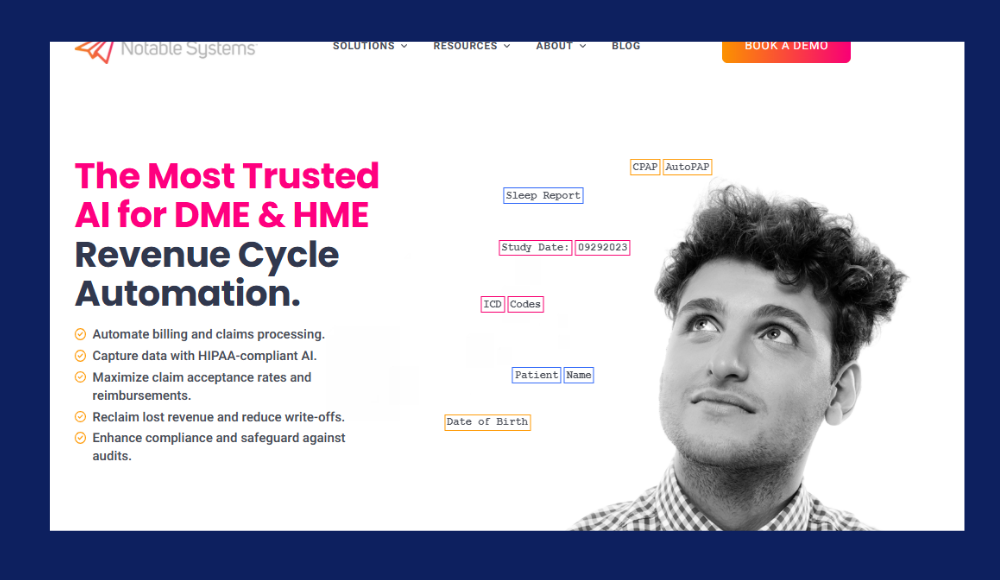
In the fast-evolving healthcare technology space, revenue cycle management (RCM) is one of the most critical yet complex functions. Notable Systems, a Denver-based startup, is tackling this challenge with AI-driven automation.
Their recent $12 million Series B funding round, co-led by Harbert Growth Partners and Grotech Ventures, positions them to expand aggressively and solidify their leadership in this niche.
What Does Notable Systems Do?
Notable Systems builds AI-powered tools that help medical equipment providers process clinical documents and claims more efficiently. Their technology converts unstructured documents — such as doctor’s notes, prescriptions, and certificates of medical necessity — into structured data ready for claim submission.
Unlike traditional RCM platforms that focus on administrative tracking or basic form filling, Notable’s system understands complex reimbursement rules, evaluates documents against insurance criteria, and automates much of the approval and billing process. This results in faster claim cycles, fewer denials, and reduced manual workload.
Industries Served
Their platform primarily serves:
- Durable Medical Equipment (DME) providers
- Home Medical Equipment (HME) providers
- Laboratory and diagnostic services
- Other post-acute care providers
These are verticals that often struggle with fragmented workflows, paper-heavy intake processes, and varied insurance policies, making them a prime fit for Notable’s automation.
Key Investors
Notable Systems’ $12 million Series B round was backed by two seasoned venture capital firms known for identifying high-growth technology companies. Their involvement not only brings capital but also strategic expertise and long-term support, helping Notable scale efficiently in a competitive market.
Harbert Growth Partners
Harbert Growth Partners, affiliated with Harbert Management Corporation, is a growth-stage investor with a strong portfolio in healthcare and enterprise software. The firm is known for backing companies with the potential to lead niche markets. As of 2025, Harbert manages over $8 billion in assets and focuses on high-impact technology solutions.
Their investment in Notable Systems highlights their confidence in AI-led transformation in the healthcare space.
Grotech Ventures
Grotech Ventures has been backing tech startups since 1984 and has invested in over 130 companies. Their focus lies in early to growth-stage companies with innovative B2B offerings. They typically invest between $500K and $5M and continue supporting portfolio companies through later rounds.
Their backing adds strategic credibility and access to long-term capital, both crucial for a company in growth mode like Notable.
Investor Perspective
Tom Roberts, General Partner at Harbert, said:
“Notable Systems is solving a massive and expensive problem in the health care system with extraordinary precision and performance. Their technology is already delivering measurable ROI for some of the largest DME providers in the country.”
This aligns with a broader trend: venture capital firms are increasingly prioritizing startups that offer tangible, measurable improvements in outdated operational systems like medical billing and claims.
How the $12M Funding Will Be Used
The $12 million Series B funding will serve as a catalyst for Notable Systems to transition from a fast-growing startup to a category leader in healthcare automation.
The funds will be strategically allocated across several key areas that align with the company’s mission to revolutionize revenue cycle management.

Scaling Operations
A significant portion of the funding will be invested in strengthening Notable’s internal infrastructure. As the client base continues to expand, the company is prioritizing team growth across engineering, onboarding, account management, and customer support. These hires will be essential for maintaining high service standards and ensuring smooth implementation for new clients. In a space where reliability is critical, operational maturity is just as important as technological innovation.
Notable will also invest in systems and processes that support a larger enterprise-scale operation. This includes tools for internal collaboration, workflow automation, and customer success tracking to ensure clients experience measurable value early and often.
Accelerating Product Development
Continued innovation is a core part of Notable’s growth strategy. The company plans to invest heavily in its R&D function to advance its AI models and extend the capabilities of its core platform. Enhancements will include more nuanced document classification, deeper learning for reimbursement pattern recognition, and faster turnaround for document-to-claim conversions.
In addition, Notable is expanding its payor-specific rulesets to cover a broader range of insurance providers and reimbursement scenarios. This is particularly important as healthcare regulations and insurance requirements vary widely across states and care types. By tailoring automation to these nuances, the platform becomes more valuable and scalable.
Deeper integrations with leading EMR and billing systems are also on the roadmap, making Notable’s solution even more plug-and-play for large providers and health systems.
Expanding Market Presence
While Notable has already gained significant traction among DME and HME providers, it sees a clear opportunity to expand into adjacent verticals. These include specialty labs, orthotics and prosthetics providers, and post-acute care organizations — all of which face similar document-heavy, compliance-sensitive RCM challenges.
The company is also eyeing geographic expansion. Within the U.S., there are still untapped regional providers with outdated systems and high operational overhead. Internationally, Notable is beginning to assess regulatory environments in select global markets where healthcare digitization is a growing priority. Early-stage market research and partnerships will lay the foundation for long-term global reach.
Building Sales and Marketing Capacity
To meet rising demand, Notable will significantly boost its sales and marketing efforts. That means scaling its go-to-market team with experienced sales professionals who understand the healthcare landscape and can guide complex buying processes.
Marketing initiatives will include brand building, thought leadership, digital campaigns, and participation in industry conferences. Notable plans to lead conversations around the future of AI in healthcare RCM — positioning itself as not just a software vendor, but a category-defining brand.
Webinars, case studies, and client success stories will be central to educating the market and demonstrating ROI. These efforts aim to accelerate pipeline growth, shorten sales cycles, and build a trusted name among healthcare leaders looking to modernize their financial operations.
Industry Context and Opportunity
The healthcare industry is under growing pressure to streamline operations, cut costs, and accelerate reimbursements. Revenue cycle management (RCM), often manual and inefficient, has become a key target for disruption.
Intelligent automation is now a must-have, not a luxury — and Notable Systems is well-positioned to lead that shift.
The RCM Problem
Healthcare providers in the U.S. spend over $200 billion annually on billing-related administrative functions. These include claims processing, collections, eligibility checks, and appeals. Most of these tasks are handled manually, which slows down reimbursements and increases the risk of errors.
For small and mid-sized providers, the burden is especially heavy. Many lack the internal resources to keep up with constantly shifting insurance rules, leading to high denial rates, delayed payments, and burned-out staff.
Manual RCM processes don’t just impact revenue. They create friction throughout the system — from longer patient wait times to increased administrative overhead and staff dissatisfaction.
Why AI and Automation Are Taking Over
Several long-term factors are pushing healthcare providers to adopt automation in RCM. These aren’t passing trends they reflect deep challenges in the system that traditional tools can’t fix.
Workforce Shortages in Billing and Administrative Roles
The healthcare industry is facing ongoing staffing shortages, particularly in non-clinical roles like billing, coding, and claims management. Hiring and retaining skilled workers is becoming increasingly difficult especially for providers operating on thin margins.
AI solutions like Notable’s provide scalability and resilience. They take over routine, time-consuming tasks so human teams can focus on exception handling and strategic work.
Regulatory Complexity and Constant Change
Insurance payors frequently update their reimbursement policies, medical necessity criteria, and documentation requirements. For billing teams, staying compliant is a moving target that requires constant oversight.
AI platforms excel here by continuously learning and updating their rulesets. Notable’s system automatically applies these changes, ensuring claims are clean and complete before submission — and drastically reducing rejections.
The Need for Faster, More Predictable Cash Flow
Post-COVID, many healthcare organizations are still recovering financially. Revenue predictability and speed have become critical. The longer it takes to get paid, the harder it is to stay solvent especially for DME and HME providers with high upfront costs.
By automating intake, validation, and claims submission, Notable helps providers get reimbursed faster and more reliably. This kind of automation shifts RCM from a cost center to a revenue enabler.
A Perfect Storm for Innovation
When workforce constraints, rising administrative costs, and regulatory overload all converge, providers are forced to rethink how they operate. That’s exactly the environment where a platform like Notable thrives.
With real-time AI validation, payor-specific logic, and proven ROI, Notable isn’t just keeping up with the demands of modern healthcare — it’s setting the new standard for what intelligent RCM should look like.
Future Trends in Healthcare RCM
The healthcare revenue cycle is evolving rapidly in response to new technologies, regulatory demands, and care delivery models. Automation and AI are no longer optional — they’re becoming foundational to how providers operate.
Here are four key trends shaping the future of RCM and the strategic direction for companies like Notable Systems.
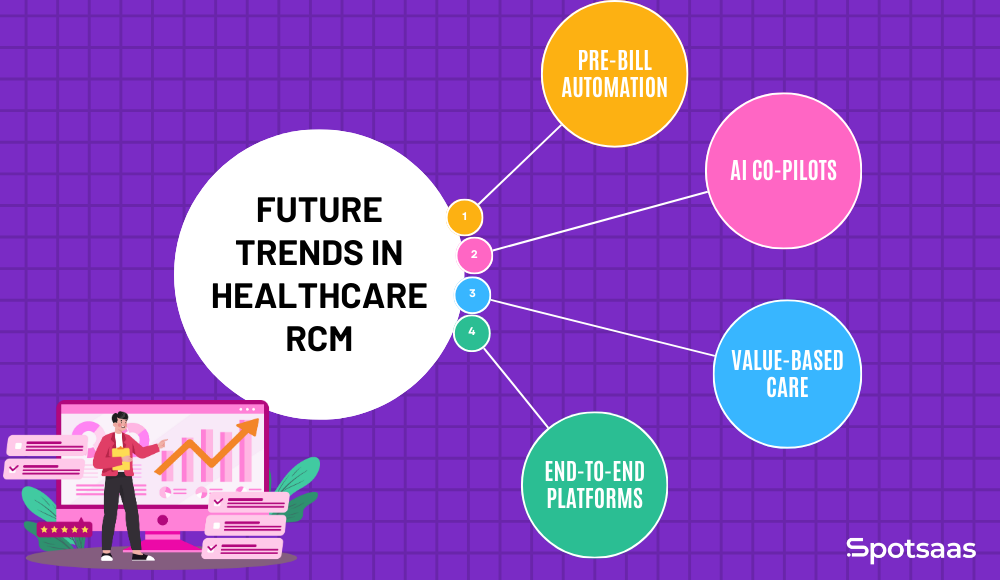
Pre-Bill Automation Will Become the Norm
The traditional RCM model focuses on fixing errors after claims are denied. But the cost and complexity of denials make that model unsustainable. More healthcare organizations are shifting toward pre-bill automation, where claims are validated for compliance, documentation, and eligibility before they’re submitted.
This shift reduces denial rates, speeds up payments, and lowers operational overhead. It’s a proactive approach that improves revenue predictability and cash flow — two critical metrics for financial health.
AI Co-Pilots for Billing Staff
As billing workflows grow more complex, AI is stepping in to assist — not replace — human staff. AI co-pilot tools are emerging to guide billing professionals through their tasks, flag missing information, suggest coding options, and monitor compliance in real time.
These tools help eliminate human error, reduce training time for new staff, and ensure consistent application of rules. Co-pilots also empower smaller teams to handle larger volumes of work without sacrificing accuracy or speed.
Shift Toward Value-Based Care
Payment models in healthcare are shifting from fee-for-service to value-based care, where reimbursement is tied to outcomes and quality. This creates new documentation and reporting challenges for providers.
Revenue cycle tools must now do more than process claims — they must capture and structure data that proves care quality, supports audits, and demonstrates compliance with value-based contracts. Platforms like Notable are already enabling this by transforming unstructured documentation into structured, searchable data ready for analysis and reporting.
Integrated End-to-End RCM Platforms Will Gain Traction
The future of RCM lies in platforms that handle the entire billing journey — from patient intake to reimbursement — without requiring dozens of disconnected tools. Providers are seeking unified systems that can manage data, automate approvals, validate claims, and track performance from a single dashboard.
Integrated RCM platforms reduce data loss, simplify compliance, and offer better visibility across departments. As AI matures, we’ll see more providers consolidate their billing tech stacks in favor of all-in-one solutions that can scale with them. Notable’s approach aligns with this trend by offering a highly modular yet end-to-end automation engine.
Conclusion
With $12 million in new funding, Notable Systems is scaling fast to tackle one of healthcare’s biggest pain points: revenue cycle inefficiency. Its AI-powered platform is built for speed, accuracy, and real-world results exactly what providers need as they shift toward automation and value-based care.
Backed by top investors and strong market traction, Notable isn’t just solving a problem — it’s reshaping how healthcare gets paid.
Stay tuned for more funding news and SaaS updates follow us for the latest insights.